Expert-Backed Tips for Daily Living with Rheumatoid Arthritis

Living with rheumatoid arthritis isn’t just about joint pain—it’s a full-body, full-life experience. People with rheumatoid arthritis face daily hurdles, from extreme fatigue that zaps energy for even simple tasks to frustrating flares that can strike without warning. Research shows that nearly two-thirds of RA patients are overweight or obese—a factor that not only accelerates disease progression but can also blunt the effects of life-changing treatments. But here’s the empowering part: daily management truly makes a difference. Simple lifestyle tweaks, like losing just 10 pounds or sticking to a self-care routine, have been shown to improve symptoms, enhance treatment response, and help patients stay active and independent. Early use of disease-modifying antirheumatic drugs (DMARDs) can tip the odds in your favor—but pairing treatment with expert-backed daily strategies is where the real magic happens. In this guide, we dive into practical, research-driven tips that actually work for living well with rheumatoid arthritis—so you can thrive, not just survive.
Quit Smoking to Reduce Inflammation
Smoking cessation stands among the most impactful lifestyle modifications available to rheumatoid arthritis patients. Currently, up to 30% of people with RA smoke, surpassing the general population’s rate of 15%. This single behavioral change can fundamentally alter disease progression and treatment responses.
Quit Smoking to Reduce Inflammation – What It Involves
Complete tobacco elimination through behavioral modification and potential medication support defines the smoking cessation process. This approach requires understanding nicotine dependence, managing withdrawal symptoms, and establishing new coping strategies. Both smoking intensity and duration directly influence RA risk and severity. Even partial reduction proves beneficial—patients unable to quit entirely but who decreased daily cigarette consumption from 12 to 6 demonstrated measurable improvements.
Quit Smoking to Reduce Inflammation – Why It Matters
Cigarette smoking operates as both a catalyst and accelerator for rheumatoid arthritis development. Research reveals that smokers exhibit significantly elevated levels of pro-inflammatory cytokines—specifically TNF-α, IL-1, and IL-6—which are proteins that drive RA disease processes. Additionally, smoking establishes a systemic proinflammatory state that directly compromises treatment effectiveness.
The clinical implications prove substantial. Smokers with RA experience:
- Diminished response to methotrexate and biologic treatments
- Elevated disease activity and joint damage
- Heightened cardiovascular risk beyond RA’s inherent elevated risk
- Decreased likelihood of achieving remission
Conversely, patients who ceased smoking witnessed their disease activity score (DAS28-CRP)—a measure of joint inflammation and tenderness—improve from 4.9 to 2.9 compared to continuing smokers. Former smokers reduced their risk of developing seropositive RA by 37% after 30 years of abstinence.
Quit Smoking to Reduce Inflammation – How to Quit
Successful cessation typically combines behavioral support with pharmacological intervention. Effective approaches include:
Healthcare provider consultation regarding nicotine replacement therapy (NRT) or medications such as varenicline/bupropion, which many insurance plans cover. Establishing a specific quit date while informing friends and family creates accountability structures. Developing alternative activities for craving management—reading, exercise, puzzles, or breathing techniques—provides support during challenging moments.
Rheumatology-specific cessation programs demonstrate 21-33% success rates after 6-24 months. Crucially, patients report that understanding the direct connection between smoking and RA provides powerful motivation—many previously remained unaware that smoking reduces medication effectiveness and accelerates joint damage.
Eat a Balanced, Nutrient-Rich Diet
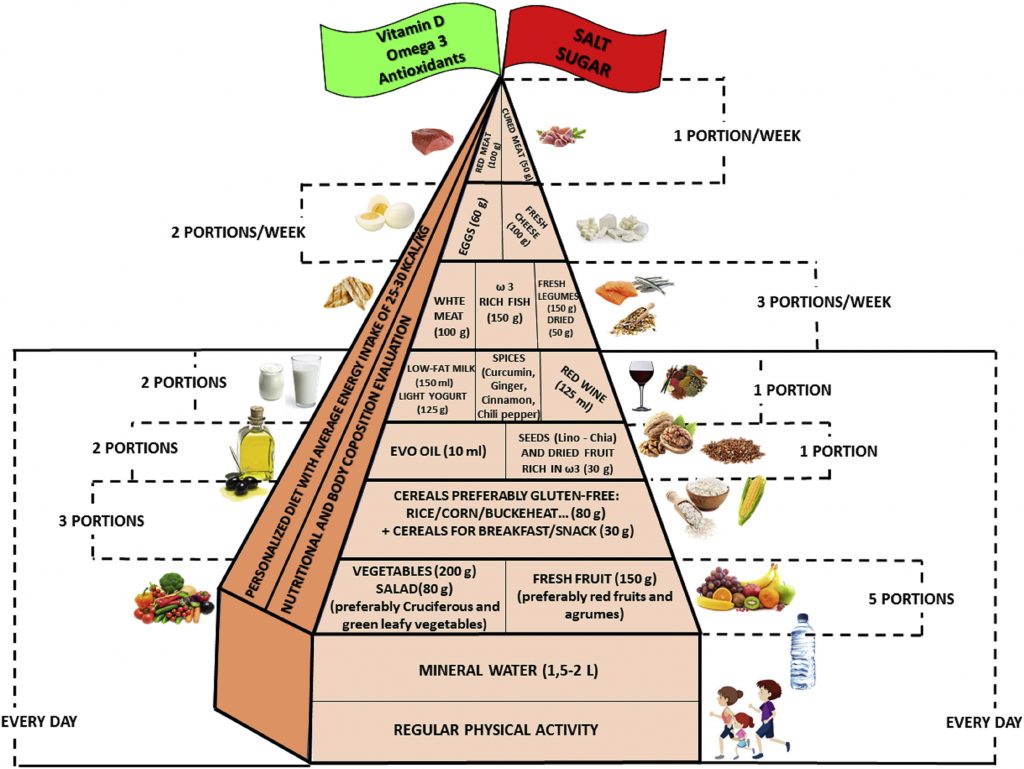
Image Source: Clinical Nutrition
Food choices wield considerable influence over rheumatoid arthritis symptoms and systemic inflammation. Specific dietary patterns can directly modify disease activity, working alongside conventional medications to enhance RA management.
Eat a Balanced, Nutrient-Rich Diet – What It Involves
The Mediterranean dietary approach forms the foundation of optimal nutrition for RA patients—emphasizing fruits, vegetables, whole grains, fish, olive oil, nuts, and seeds. This eating pattern focuses on:
- Antioxidant-rich foods from vibrant fruits and vegetables (targeting 4+ vegetable servings and 2+ fruit servings daily)
- Omega-3 fatty acids from fatty fish such as salmon, mackerel, and sardines, plus plant sources like walnuts
- Whole grains rather than processed carbohydrates
- Lean protein sources including fish, poultry, and legumes
- Beneficial fats especially extra-virgin olive oil
This approach deliberately reduces processed foods, added sugars, and saturated fats that fuel inflammatory processes.
Eat a Balanced, Nutrient-Rich Diet – Why It Matters
Nutrition directly affects RA symptoms through multiple pathways. Mediterranean-style eating patterns demonstrate measurable reductions in inflammation while improving joint pain and morning stiffness. Women with RA following this diet for merely six weeks showed significantly decreased joint pain compared to control participants.
Certain foods contain active anti-inflammatory compounds. Omega-3 fatty acids found in fish help diminish RA pain, swelling, and stiffness. Fiber-rich legumes can lower C-reactive protein (CRP)—a blood marker indicating inflammation levels throughout the body.
Antioxidants present in fruits and vegetables combat free radicals that potentially damage joint tissues and exacerbate RA symptoms. A nutrient-dense diet therefore supports disease management while addressing common nutritional deficiencies in RA patients, particularly calcium, vitamin D, and antioxidants.
Eat a Balanced, Nutrient-Rich Diet – How to Start
Start by gradually increasing plant-based foods in your meals. Initially focus on incorporating more colorful fruits and vegetables, especially those containing vitamin C such as berries, citrus fruits, and peppers.
Next, add omega-3 sources—begin with fatty fish twice weekly. Substitute refined grains with whole grain alternatives and transition to olive oil as your primary cooking fat.
Maintain a food diary to identify potential trigger foods, since some individuals may experience symptom flares with certain items. Remember that dietary modifications support rather than replace prescribed medications—always discuss significant dietary changes with your rheumatologist before implementation.
Practice Tai Chi or Yoga
“Remember there is absolutely hope for a pain free, active, healthy life, even with RA, remain active, move even when it hurts. Meditation and yoga are very underrated to combat physical and mental pain.” — Deeper from New Jersey (RA patient advocate), Patient advocate, sharing lived experience and advice for RA management
Image Source: Just Breathe Tai Chi
“Remember there is absolutely hope for a pain free, active, healthy life, even with RA, remain active, move even when it hurts. Meditation and yoga are very underrated to combat physical and mental pain.” — Deeper from New Jersey (RA patient advocate), Patient advocate, sharing lived experience and advice for RA management
Mind-body practices rooted in ancient traditions provide distinctive advantages for individuals managing rheumatoid arthritis. Tai chi and yoga merge gentle physical movements with mindfulness principles, offering therapeutic benefits where traditional exercise approaches might trigger joint discomfort.
Practice Tai Chi or Yoga – What It Involves
Tai chi emerged from ancient Chinese martial arts, characterized by slow, flowing movements that transition seamlessly between postures. This discipline integrates deep diaphragmatic breathing with relaxation techniques and deliberate, controlled movements while emphasizing proper postural alignment. Yoga, which developed within ancient Indian traditions, represents a holistic system incorporating physical postures (called asanas), controlled breathing methods, and meditative practices. Both approaches emphasize the mind-body connection, creating an integrated framework for physical activity.
Practice Tai Chi or Yoga – Why It Matters
These time-tested practices offer measurable benefits for rheumatoid arthritis management. Research demonstrates that tai chi enhances flexibility, builds muscle strength, and helps maintain overall fitness levels. Additionally, studies indicate that tai chi practice reduces pain intensity, improves balance, and enhances quality of life measures.
Yoga yields comparable therapeutic effects for RA patients. A focused study revealed that yoga practice may enhance physical function, reduce disease activity, and improve grip strength. Further research showed that after 12 weeks of practice, yoga participants experienced improvements in fatigue levels and mood regulation. Both practices address psychological dimensions of chronic pain management—alleviating stress, anxiety, and depressive symptoms frequently experienced alongside rheumatoid arthritis.
Practice Tai Chi or Yoga – How to Begin
Begin with modified movements tailored to your current physical capabilities. Dr. Paul Lam, a family physician who developed arthritis during his teenage years, observes that “A lot of people with arthritis don’t know they can do tai chi”. Specialized programs designed for arthritis patients are available, including the “Tai Chi for Arthritis” program which features 12 adapted Sun-style movements.
When exploring yoga, seek instructors with arthritis experience. Robin Rothenberg, a certified yoga specialist, recommends avoiding “power yoga, hot yoga, and flow (also known as Vinyasa yoga), which can increase internal heat and put excessive pressure on the joints”. Suitable beginning postures include gentle forward folds, cobra pose, seated spinal twists, and bridge pose.
Currently, DVDs, online programs, and community classes designed specifically for arthritis patients are readily accessible through organizations such as the Arthritis Foundation.
Use Assistive Devices for Daily Tasks

Image Source: Everyday Health
Daily activities that once seemed effortless can become formidable challenges when rheumatoid arthritis affects joint function and mobility. Assistive devices—specialized tools designed to reduce joint stress—serve as practical solutions for these everyday obstacles. Research shows that approximately two-thirds of people with arthritis incorporate these adaptive tools into their daily routines, establishing them as fundamental components of effective RA management.
Use Assistive Devices for Daily Tasks – What It Involves
Assistive devices, also termed adaptive equipment, represent specialized tools engineered to minimize joint stress while simplifying routine activities. These solutions span from basic kitchen implements to comprehensive bathroom modifications. The primary categories include:
- Personal care items – Button hooks, zipper pulls, long-handled shoehorns, and built-up handles for toothbrushes
- Kitchen tools – Jar openers, ergonomic utensils, two-handled pots, and electric can openers
- Mobility aids – Canes, reachers, and grabbing tools
- Home modifications – Lever door handles, raised toilet seats, and shower grab bars
Use Assistive Devices for Daily Tasks – Why It Matters
These tools serve a dual purpose: protecting joints from excessive stress while maintaining personal independence. Without appropriate adaptive equipment, many individuals gradually relinquish activities they previously enjoyed, often without conscious awareness of this process.
Clinical studies indicate that early RA patients typically utilize between three (men) to five (women) assistive devices, with eating and drinking activities representing the most common applications. Individuals with severe RA may employ up to ten devices regularly. Beyond preserving independence, these tools demonstrate measurable benefits in pain reduction, fatigue management, and overall quality of life enhancement.
Use Assistive Devices for Daily Tasks – How to Choose Them
Selecting appropriate devices requires careful assessment of individual needs and specific challenges. Healthcare professionals—including physicians, occupational therapists, or physical therapists—can provide targeted recommendations based on your particular condition.
When evaluating potential devices, assess whether each tool effectively reduces pain and joint stress, minimizes energy expenditure, provides convenience, and offers adequate stability for hypermobile joints.
Assistive devices are accessible through medical supply stores, pharmacies, and online retailers across various price ranges. Insurance coverage varies significantly, so verification with your provider is essential—items classified as medical equipment (such as bed risers or bath benches) may qualify for coverage, while general household items typically do not. For individuals without insurance coverage, doctor’s offices or Federally Qualified Health Centers may offer essential items at reduced costs.
Apply the 4 Ps of Energy Conservation
Image Source: Frontiers
Fatigue presents one of the most challenging aspects of living with rheumatoid arthritis, often leaving patients feeling drained before the day begins. The 4 Ps methodology—Problem-solving, Planning, Prioritizing, and Pacing—provides a structured framework for managing limited energy resources throughout daily activities.
Apply the 4 Ps of Energy Conservation – What It Involves
This systematic approach addresses energy depletion through four distinct components:
- Problem-solving: Examining daily routines to identify activities that trigger pain, discomfort, or excessive fatigue. This process involves analyzing which specific tasks or body positions contribute most significantly to energy depletion.
- Planning: Developing intentional schedules that balance demanding activities with adequate rest periods. This includes creating visual calendars—often color-coded for clarity—that map out both activities and recovery breaks throughout the week.
- Prioritizing: Distinguishing between essential and optional tasks through honest assessment. This step requires evaluating which activities must be completed immediately, which can be postponed, and which might be delegated to others.
- Pacing: Dividing larger tasks into smaller, manageable segments with scheduled rest intervals. This approach prevents exhaustion by stopping activities before fatigue overwhelms the system.
Apply the 4 Ps of Energy Conservation – Why It Matters
Energy conservation directly influences rheumatoid arthritis management outcomes. Proper pacing allows inflamed joints adequate time to rest and repair, thereby reducing inflammation and preventing overuse injuries. Balanced activity schedules help maintain steady energy levels throughout the day, avoiding the destructive “boom and bust” pattern where excessive activity leads to prolonged recovery periods.
Strategic energy management enables participation in meaningful activities rather than exhausting all available resources on routine obligations. This balanced approach supports psychological well-being alongside physical health.
Apply the 4 Ps of Energy Conservation – How to Use Them
Start by monitoring current energy patterns and identifying peak performance times. Schedule demanding activities during these optimal periods. Create visual planning tools using calendars or charts, with activities marked in one color and rest periods in another.
When prioritizing tasks, develop daily lists ranked by importance. Ask yourself: “Does this require completion today?”, “Does it need to be done at all?”, and “Can someone else assist with this task?”.
For pacing strategies, apply the “Two Hour Pain Rule”—if discomfort persists beyond two hours after an activity, you likely exceeded your limits and should reduce intensity next time. Alternate between sitting, standing, and walking throughout the day to prevent overstraining specific muscle groups.
Remember that energy conservation focuses on strategic resource allocation rather than simply reducing activity—the goal is enabling greater participation in valued activities.
Get Regular Medical Reviews
Professional medical oversight represents a fundamental pillar in effective rheumatoid arthritis management. Consistent monitoring enables healthcare providers to optimize treatment plans while patients maintain their self-care practices.
Get Regular Medical Reviews – What It Involves
Rheumatoid arthritis medical reviews typically follow a structured schedule—annual assessments serve as baseline evaluations, while active disease requires monthly monitoring. Patients experiencing symptom fluctuations benefit from monthly appointments where healthcare providers can modify medications, evaluate side effects, and offer clinical support. Once therapeutic targets are achieved, follow-up appointments at six-month intervals help ensure sustained remission.
Standard review appointments encompass several key components:
- Joint examination to assess active inflammation
- Medication review including current therapies and potential adverse effects
- Evaluation of systemic health concerns and comorbid conditions
- Laboratory testing to monitor inflammatory markers and medication effects
- Imaging studies such as radiographs or ultrasound to track disease progression
Get Regular Medical Reviews – Why It Matters
Consistent medical supervision provides critical benefits throughout the disease course. These appointments serve as early warning systems, identifying disease flares before irreversible joint damage occurs. Regular monitoring also facilitates prompt therapeutic adjustments when current treatments lose effectiveness.
Medical reviews extend beyond joint health to encompass systemic complications. Healthcare providers screen for RA-related complications affecting cardiovascular, pulmonary, and ocular systems. Research demonstrates that patients receiving regular rheumatologic care experience superior clinical outcomes. Monthly monitoring during active disease phases proves particularly valuable for treatment optimization, allowing for medication dose adjustments and short-term corticosteroid management.
Get Regular Medical Reviews – How to Prepare
Thorough preparation maximizes the value of specialist appointments. Document symptoms between visits, recording pain intensity, potential triggers, and medication responses. Schedule required laboratory work 1-2 weeks prior to appointments, ensuring results are available for clinical discussion.
Develop a prioritized question list, organizing concerns by clinical importance. Rheumatologists depend heavily on detailed patient histories, so prepare specific information regarding:
- Symptom onset and progression patterns
- Factors that ameliorate or exacerbate symptoms
- Morning stiffness duration and severity
- Location and characteristics of joint swelling
Compile a complete medication inventory including dosages, administration schedules, and over-the-counter supplements. Consider bringing a trusted companion who can assist with information retention during the appointment.
Improve Your Sleep Hygiene
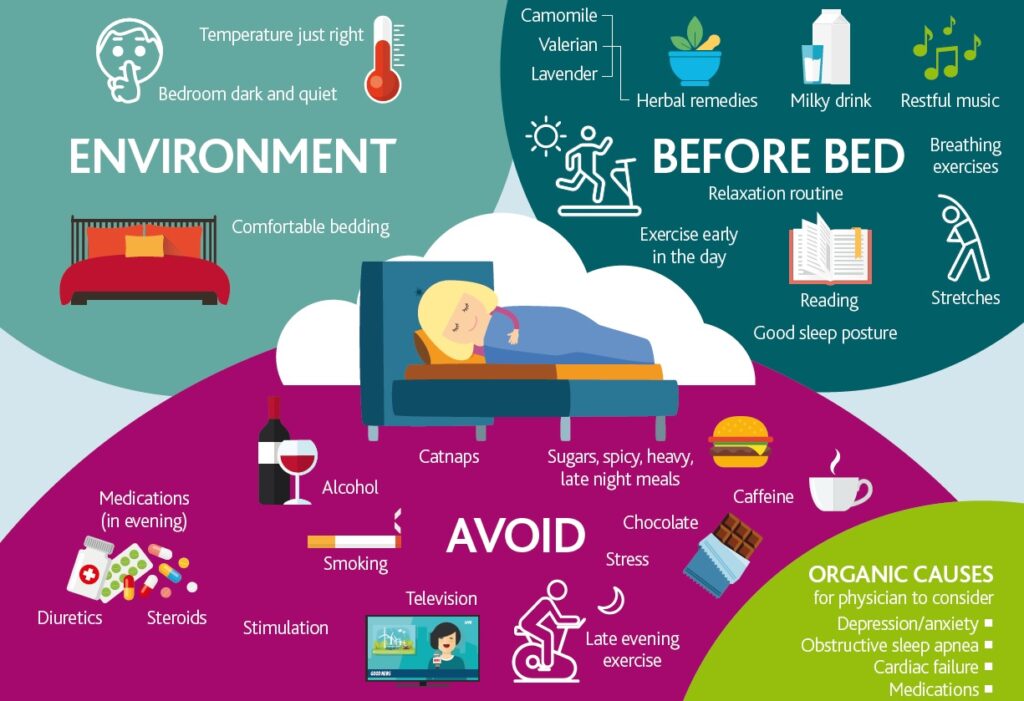
Image Source: NRAS
Sleep disturbances plague up to 80% of people with arthritis. This overwhelming statistic reveals a fundamental challenge: poor sleep doesn’t simply leave patients feeling tired—it actively worsens disease symptoms, creating a vicious cycle where pain disrupts rest, and inadequate rest amplifies pain sensitivity.
Improve Your Sleep Hygiene – What It Involves
Sleep hygiene refers to a collection of behavioral practices and environmental adjustments designed to promote consistent, restorative sleep. These practices include maintaining regular bedtimes and wake times, optimizing bedroom conditions for rest, and developing pre-sleep routines that signal the body to prepare for recovery. When implemented consistently, these measures help establish what sleep specialists call an “internal snooze clock”—the body’s natural circadian rhythm that regulates sleep-wake cycles.
Improve Your Sleep Hygiene – Why It Matters
Sleep and rheumatoid arthritis exist in a bidirectional relationship, meaning each condition influences the other. Pain naturally interferes with sleep onset and maintenance, yet sleep deprivation simultaneously heightens pain perception. Research reveals that sleep-deprived individuals show increased activity in brain regions responsible for pain processing, making them more sensitive to discomfort than well-rested counterparts.
This relationship extends beyond immediate comfort. Chronic sleep disruption contributes to systemic inflammation, intensifies fatigue, increases depressive symptoms, and diminishes daily functioning capacity. For individuals already managing the inflammatory burden of rheumatoid arthritis, poor sleep compounds these challenges significantly.
Improve Your Sleep Hygiene – How to Improve It
Several evidence-based strategies can help break the pain-sleep disruption cycle:
- Maintain schedule consistency – Retire to bed and wake at identical times daily, including weekends, to strengthen your body’s natural rhythm
- Optimize your sleep environment – Keep bedrooms quiet, dark, cool, and reserved exclusively for sleep—avoid work, television, or other stimulating activities
- Control stimulant exposure – Eliminate caffeine after midday, reduce evening fluid consumption, and avoid alcohol before bedtime
- Limit blue light exposure – Power down electronic devices at least one hour before sleep, as artificial light disrupts melatonin production
- Address pain preemptively – Apply cold compresses to inflamed joints or use heating pads before bedtime to reduce discomfort
Persistent sleep difficulties may indicate underlying conditions like sleep apnea or restless leg syndrome. Sleep specialists can conduct overnight studies to identify these issues. Treating such conditions often produces remarkable improvements in both sleep quality and arthritis symptom management.
Take Care of Your Dental Health

Image Source: CreakyJoints Australia
Research reveals a troubling pattern: people with rheumatoid arthritis face significantly higher rates of periodontal disease and tooth loss. This connection extends far beyond mere coincidence, representing a complex bidirectional relationship that demands careful attention in RA management.
Take Care of Your Dental Health – What It Involves
Dental care for individuals with rheumatoid arthritis requires addressing both standard oral hygiene needs and RA-specific challenges. Common oral complications include periodontal disease (gum disease), temporomandibular joint dysfunction affecting jaw movement, and xerostomia (dry mouth). Since RA triggers systemic inflammation throughout the body, oral tissues become vulnerable to this same inflammatory process.
The approach encompasses regular professional dental evaluations, modified daily hygiene routines, and proactive management of RA-related oral symptoms. Patients often need specialized tools and techniques to accommodate joint limitations while maintaining effective oral care.
Take Care of Your Dental Health – Why It Matters
The relationship between oral health and rheumatoid arthritis operates through shared inflammatory pathways. Studies demonstrate that RA patients experience elevated rates of dental caries, pulpitis (tooth nerve inflammation), gingivitis, and oral ulceration.
Sjögren’s syndrome, which frequently accompanies RA, can severely damage salivary glands. This leads to profound oral dryness, difficulty eating, and potentially tooth loss. Saliva contains protective proteins that naturally reduce harmful mouth bacteria—without adequate saliva production, tooth decay risk increases substantially. Moreover, inflammation from gum disease may potentially exacerbate RA symptoms, creating a cycle of worsening health outcomes.
Take Care of Your Dental Health – How to Maintain It
Individuals experiencing hand joint pain can implement these practical adaptations:
- Electric toothbrushes with enlarged handles reduce grip strain
- Floss holders or water flossers eliminate the need for traditional flossing techniques
- Toothpaste pumps minimize hand stress compared to tube manipulation
Combat dry mouth by using sugar-free lozenges or candies to stimulate saliva production. Following brushing, apply fluoride rinses like ACT or alcohol-free mouthwashes such as Biotene.
Schedule regular dental appointments and inform your dentist about your RA diagnosis and current medications. Avoid tobacco products, which significantly worsen oral health conditions. These targeted strategies help maintain oral health despite the unique challenges posed by rheumatoid arthritis.
Balance Rest and Activity
Achieving proper equilibrium between movement and rest stands as a cornerstone principle in rheumatoid arthritis management. This careful balance protects joints from damage while preserving functional capacity and overall quality of life.
Balance Rest and Activity – What It Involves
Effective rest-activity balance demands mindful body awareness combined with strategic daily planning. The approach centers on alternating between periods of purposeful movement and structured rest intervals throughout each day. During active flare-ups, patients require increased rest to minimize inflammation, pain, and fatigue, while periods of symptom remission allow for greater activity levels. Short, frequent rest breaks provide more benefit than prolonged bed rest. The strategy encompasses more than simple alternation—thoughtful distribution of various activity types proves essential, with many individuals finding shorter exercise sessions more manageable than single extended periods, particularly during flares.
Balance Rest and Activity – Why It Matters
This equilibrium holds profound significance for long-term joint health. Insufficient rest places additional stress on already inflamed joints, potentially accelerating inflammation and structural damage. Conversely, excessive inactivity results in joint stiffness, muscle weakness, and diminished mobility. Research confirms that appropriate physical activity actually protects joints by strengthening surrounding musculature while supporting healthy weight maintenance. This balance also prevents the exhausting cycle of overexertion followed by lengthy recovery periods. Those who achieve this equilibrium frequently report enhanced physical and mental well-being.
Balance Rest and Activity – How to Practice It
Successful implementation requires individualized strategies:
- Monitor body signals carefully – Pain or fatigue lasting beyond two hours post-activity suggests overexertion
- Time activities strategically – Schedule exercise when pain levels are lowest and medication effectiveness peaks
- Divide activities into segments – Consider three 10-minute sessions instead of one 30-minute session during flares
- Rotate activity types – Alternate between sitting, standing, and walking tasks to prevent continuous strain on identical joints
- Choose gentle movement options – Walking, swimming, or gardening often provide mobility benefits without excessive joint stress
Beyond physical considerations, psychological adaptation plays an important role. Accepting that chronic illness creates variable daily experiences—some days allowing increased activity while others requiring additional rest—forms part of effective management. Consistent application of these principles often leads to improved functionality and reduced symptom severity.
Use Ergonomic Furniture and Tools
Workplace challenges intensify for individuals managing rheumatoid arthritis, where poor positioning can transform routine tasks into sources of pain and joint strain. Ergonomic modifications to workspaces and everyday tools provide substantial relief while promoting independence in daily activities.
Use Ergonomic Furniture and Tools – What It Involves
Ergonomic adaptations center on achieving optimal body positioning that minimizes stress on affected joints. This specialized approach involves selecting supportive seating, positioning computer equipment correctly, and incorporating tools designed for easier grip and reduced strain. A properly configured ergonomic workspace features a chair with lumbar support (lower back support), adjustable height settings, and a stable five-point base for safety.
Additional supportive equipment includes document holders positioned at eye level, laptop risers, and hands-free telephone headsets that promote proper posture maintenance. Computer users benefit particularly from ergonomic keyboards and vertical mice that maintain hands and forearms in neutral positions—especially valuable for those experiencing carpal tunnel syndrome, a condition that commonly occurs alongside RA.
Use Ergonomic Furniture and Tools – Why It Matters
Proper ergonomic setup directly influences joint health and pain intensity. Without adequate support, people often unconsciously adopt harmful postures that increase inflammation and accelerate joint damage over time. Correctly positioned equipment helps maintain the spine’s natural curve while keeping joints in neutral alignment—meaning they’re positioned in their most comfortable, stress-free state.
Studies demonstrate that properly arranged workstations significantly reduce neck, shoulder, and back strain commonly experienced by RA patients. Under the Americans with Disabilities Act, many workers possess legal rights to request workplace accommodations for these necessary adjustments, making ergonomic modifications both medically beneficial and legally supported.
Use Ergonomic Furniture and Tools – How to Set It Up
Start by selecting a chair that provides lumbar support and allows comfortable sitting with your back fully against it. Ensure your feet reach the floor comfortably, with knees positioned slightly higher than your hips. Position your computer monitor 20-26 inches from your body, with the screen top aligned with your head in a neutral position.
Maintain arms at 90-degree angles while typing, keeping wrists relaxed and straight. Consider consulting an occupational therapist for personalized ergonomic assessment tailored to your specific needs and limitations. For extensive laptop users, a separate keyboard and laptop riser become essential to prevent neck strain from looking down at the screen.
Remember that proper ergonomics extends beyond work environments—apply these same principles to home furniture and everyday tools throughout your living space.
Stay Emotionally Resilient
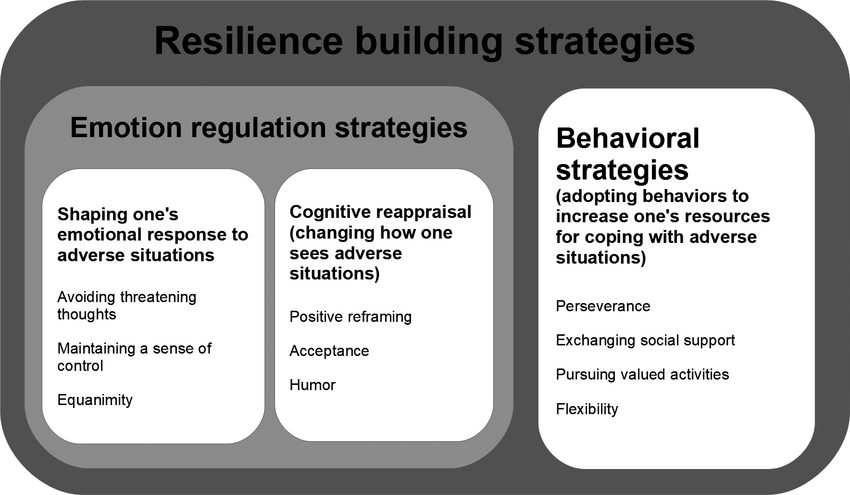
Image Source: ResearchGate
Mental health challenges affect people with rheumatoid arthritis at alarming rates. Depression occurs nearly three times more frequently in RA patients compared to the general population, yet this crucial aspect of care often remains overlooked in treatment approaches.
Stay Emotionally Resilient – What It Involves
Emotional resilience involves cultivating psychological strength to handle the unpredictable nature of rheumatoid arthritis. This encompasses developing effective coping strategies for pain management, addressing concerns about disease progression, and preserving social relationships despite physical constraints. Resilience means building the capacity to bounce back from challenges—whether managing symptom flares or adjusting to new limitations. Dr. Robert Wicks describes resilience as “the difference between making arthritis one part of your story and allowing it to be your entire narrative”.
Stay Emotionally Resilient – Why It Matters
Emotional health and RA influence each other through complex pathways. Chronic inflammation disrupts normal stress responses, potentially triggering depression, which subsequently worsens long-term RA outcomes. Untreated depression may interfere with medication adherence and self-management practices. Physiologically, stress hormones and neurochemicals—including cortisol, serotonin, and norepinephrine—directly influence mood and behavior patterns. Studies demonstrate that individuals with greater resilience recover more quickly, handle pain more effectively, and achieve better overall health outcomes.
Stay Emotionally Resilient – How to Build It
Evidence-based strategies can help strengthen emotional resilience:
- Connect with support networks – Join others who understand your experience through in-person or online support groups
- Explore professional treatment – Cognitive Behavioral Therapy (CBT) significantly reduces anxiety, depression, and fatigue in RA patients
- Develop mindfulness practices – Regular mindfulness and meditation can decrease stress, anxiety, and even disease activity
- Cultivate gratitude – People who practice gratitude regularly report feeling more connected, optimistic, and resilient
- Focus on possibilities – Concentrate on capabilities rather than limitations; resilient individuals ask “How can I improve my situation?”
Emotional fluctuations are normal when living with RA, but mental health support should be viewed as an essential component of comprehensive care. Simple practices like deep breathing exercises or maintaining social connections can significantly enhance your ability to manage daily challenges.
Track Your Symptoms and Triggers
“Check your diet and journal every day, things that you put in your mouth and the reaction the next day.” — Ashley (RA patient advocate), Patient advocate, sharing practical daily management tips for RA
Detailed symptom documentation functions as a crucial component within rheumatoid arthritis management strategies. Maintaining comprehensive records of symptoms, potential triggers, and treatment responses enables patients to assume greater control over their condition through evidence-based insights.
Track Your Symptoms and Triggers – What It Involves
Symptom tracking demands consistent documentation of essential aspects related to your RA experience. This process includes recording pain intensity using numerical scales, marking painful areas on body diagrams, noting joint swelling locations, and measuring morning stiffness duration. Beyond pain documentation, thorough tracking encompasses medication intake, fatigue levels, mobility limitations, sleep quality, stress levels, and potential triggers such as weather changes. Many patients record details multiple times daily to capture symptom fluctuations. The tracking process can utilize specialized mobile applications, digital diaries, or traditional paper journals specifically designed for arthritis symptom monitoring.
Track Your Symptoms and Triggers – Why It Matters
Accurate symptom tracking fundamentally changes doctor-patient interactions by providing objective evidence rather than relying solely on memory recall. Research demonstrates that consistent tracking helps identify patterns between activities and symptom flares. Consequently, physicians can make more informed treatment decisions—possibly switching therapies when patients report frequent flares. One patient noted, “Because I was tracking and could see patterns emerge, we could make decisions more easily”. Additionally, tracking reveals the proportion of good versus difficult days each month, offering perspective on overall disease management. This evidence-based approach empowers patients by providing concrete data to discuss with healthcare providers.
Track Your Symptoms and Triggers – How to Do It
Start by selecting a tracking method that fits your lifestyle:
- Digital apps – Options like PainScale, MyRA, and ArthritisPower offer features such as pain intensity sliders, symptom catalogs, and automatic weather data recording
- Paper journals – Structured diaries with body diagrams let you mark painful areas with X’s
- Track key elements – Document:
- Pain location and intensity
- Morning stiffness duration
- Medication effectiveness
- Potential triggers (stress, weather, food, activity levels)
- Mood and fatigue levels
Share tracking reports with your rheumatologist during appointments. Consistently recording data over time creates valuable insights about your unique RA patterns. Through systematic monitoring, you gain greater control over your condition and enhance your ability to self-manage effectively.
Communicate Openly with Your Doctor

Image Source: CreakyJoints
Patient-physician communication serves as the foundation for effective rheumatoid arthritis care. Despite this importance, a significant gap exists between patient needs and current communication practices in rheumatology settings.
Communicate Openly with Your Doctor – What It Involves
Effective physician communication encompasses honest discussions about treatment goals, symptom changes, medication concerns, and quality-of-life issues. While 84% of patients report satisfaction with their physician communication, 55% still desire more discussion about their RA treatment and goals. Physicians typically discuss health-related quality of life issues (93%), side effects/symptoms (93%), RA treatment (86%), and access/cost-related issues (63%) with their patients. However, only 8% of patients report being asked about treatment goals by their physicians. This communication requires active participation from both parties in discussing all aspects of care.
Communicate Openly with Your Doctor – Why It Matters
Patient-physician dialogue directly influences health outcomes. Research reveals that patients who feel comfortable raising concerns with their physician are more likely to describe their health as good/excellent than those who feel uncomfortable (37% vs. 27%). Effective communication helps identify treatment strategies, disease activity factors, and contributes to overall patient satisfaction.
Despite these benefits, 61% of patients feel uncomfortable raising concerns with their physician. Common barriers include believing “the physician knows best” (32%), worrying about being labeled as difficult (31%), feeling time-constrained (21%), or lacking knowledge (14%). These communication barriers can significantly impact treatment effectiveness and patient outcomes.
Communicate Openly with Your Doctor – How to Improve It
Several evidence-based approaches can enhance doctor-patient communication:
- Prepare thoroughly – Before appointments, create a prioritized list of questions and concerns. Track symptoms in a journal and bring medication lists including dosages and frequency.
- Use the “Ask Me Three” technique – End each visit by asking: “What is my main problem?”, “What do I need to do?”, and “Why is it important for me to do this?”
- Bring support – Consider having a trusted friend or family member attend appointments to take notes or record the conversation with permission
- Communicate treatment preferences – Discuss your goals openly, as physicians and patients don’t always share the same treatment priorities
Healthcare professionals respect your input and value honest discussions about all aspects of your condition, treatment responses, and concerns. This collaborative approach enables more personalized and effective care planning.
Stay Informed About RA Treatments
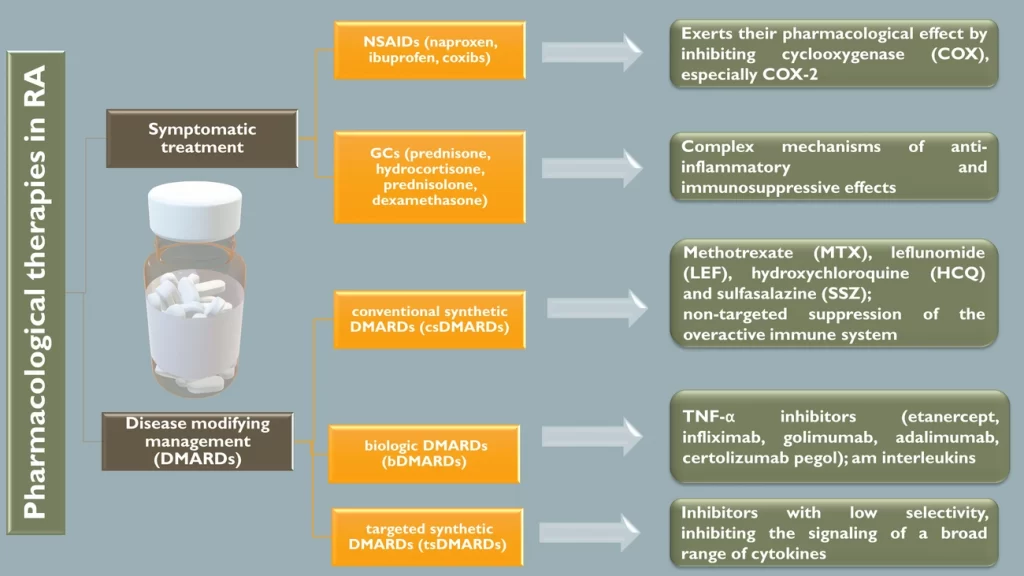
Image Source: MDPI
Knowledge about rheumatoid arthritis treatments has become increasingly crucial as therapeutic approaches evolve toward earlier, more targeted interventions. Treatment strategies now emphasize prompt use of disease-modifying drugs, making patient understanding of available options essential for achieving optimal outcomes.
Stay Informed About RA Treatments – What It Involves
Understanding RA treatments means grasping the fundamental medication categories and their mechanisms of action. Rheumatoid arthritis medications currently encompass several distinct classes: non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, conventional disease-modifying antirheumatic drugs (DMARDs), biologics, and Janus kinase (JAK) inhibitors. JAK inhibitors—including Rinvoq, Olumiant, and Xeljanz—represent the newest therapeutic class, functioning by blocking specific enzymes that fuel inflammatory processes. Emerging research investigates promising approaches such as tolerogenic dendritic cell therapy, which aims to modulate overactive immune responses.
Stay Informed About RA Treatments – Why It Matters
Treatment knowledge directly influences health outcomes for people with rheumatoid arthritis. Early therapeutic intervention with appropriate medications prevents irreversible joint damage that commonly develops within the initial two years of disease onset. Additionally, understanding how medications work enables patients to recognize potential adverse effects—baricitinib, for example, carries a boxed warning regarding thrombosis risk that requires patient monitoring. Patients who comprehend their medications’ benefits and risks can participate more effectively in treatment decisions with their healthcare providers.
Stay Informed About RA Treatments – How to Stay Updated
Several strategies can help maintain current knowledge about RA treatments:
- Access trusted sources like the Arthritis Foundation or American College of Rheumatology for evidence-based information
- Explore clinical trial participation—visit clinicaltrials.gov to locate studies accepting participants in your area
- Follow rheumatology journals or their patient-focused newsletters
- Connect with patient advocacy organizations that disseminate treatment updates
- Prepare targeted questions about emerging treatments before rheumatology appointments
Maintaining current awareness about treatment options offers both practical advantages and psychological benefits, enabling effective collaboration with your healthcare team throughout your RA journey.
Celebrate Small Wins and Progress
The psychological toll of rheumatoid arthritis extends beyond physical symptoms, often overshadowing daily accomplishments that deserve recognition. Acknowledging incremental progress forms a cornerstone of psychological resilience for those managing chronic autoimmune conditions.
Celebrate Small Wins and Progress – What It Involves
Recognition of small achievements involves consciously documenting daily accomplishments that might otherwise disappear into the routine of chronic illness management. This psychological practice encompasses acknowledging basic tasks—from completing morning routines to maintaining medication adherence—as meaningful victories. The “penny jar” visualization technique offers a tangible approach: mentally adding a penny to an imaginary jar each time you complete even minor tasks. Over time, this accumulated progress becomes visible and motivating. Additionally, this approach requires breaking larger objectives into smaller, achievable segments that remain realistic during symptom flares.
Celebrate Small Wins and Progress – Why It Matters
Rheumatoid arthritis creates unique psychological challenges where routine activities demand considerable effort. RA-related fatigue alone can disrupt carefully planned daily schedules. However, acknowledging small accomplishments provides measurable psychological benefits—enhanced self-confidence, improved energy levels, better focus, increased drive, and sustained motivation. This recognition process helps patients develop what researchers term “realistic optimism” or “fighting spirit”—psychological attitudes linked to improved medication adherence and extended survival outcomes. Moreover, celebrating incremental achievements builds resilience by emphasizing adaptability over mere productivity measures.
Celebrate Small Wins and Progress – How to Practice It
Several evidence-based strategies can help incorporate this approach into daily life:
- Reframe your perspective – Replace self-criticism with adaptability recognition, using phrases like “Look how well I adapted” rather than “I shouldn’t get so tired”
- Develop visual tracking – Create either imaginary or physical penny jars to monitor accomplishments tangibly
- Practice gratitude regularly – Research demonstrates that people with chronic illnesses who express gratitude experience lower depression rates
- Acknowledge the process – Celebrate progress throughout the journey, not just final outcomes—even when achieving targets requires extended timelines
- Recognize fundamental victories – Understand that getting out of bed during difficult mornings deserves celebration, particularly when managing chronic pain
This psychological shift transcends simple positive thinking—it represents a practical tool for maintaining motivation throughout the extended timeline of rheumatoid arthritis management.
Comparison Table
| Management Strategy | What It Involves | Key Benefits | Implementation Steps | Evidence/Research Support |
|---|---|---|---|---|
| Quit Smoking | Complete elimination of tobacco use through behavioral changes and medication support | Reduces inflammation, improves treatment effectiveness, lowers disease activity | 1. Consult healthcare providers about NRT/medications 2. Select quit date 3. Develop alternative coping activities | Patients who quit saw disease activity score improve from 4.9 to 2.9; Former smokers reduced seropositive RA risk by 37% after 30 years |
| Balanced Diet | Mediterranean-style eating pattern with emphasis on fruits, vegetables, whole grains, fish, olive oil | Reduces inflammation, improves joint pain and morning stiffness | 1. Increase plant foods gradually 2. Add fatty fish twice weekly 3. Switch to whole grains 4. Keep food journal | Women following Mediterranean diet for 6 weeks experienced reduced joint pain compared to control groups |
| Tai Chi/Yoga | Gentle movements combined with mindfulness and breathing techniques | Improves flexibility, strength, balance, and reduces pain | 1. Start with modified movements 2. Seek instructors experienced with arthritis 3. Avoid high-intensity styles | Studies show improved physical function, disease activity, grip strength, and fatigue after 12 weeks |
| Assistive Devices | Specialized tools designed to reduce joint stress in daily activities | Protects joints, preserves independence, reduces pain and fatigue | 1. Consult healthcare professionals 2. Evaluate based on individual needs 3. Check insurance coverage | Studies show 2/3 of arthritis patients use adaptive tools daily; Early RA patients typically use 3-5 devices |
| 4 Ps Energy Conservation | Problem-solving, Planning, Prioritizing, and Pacing approach | Prevents exhaustion, reduces inflammation, enables participation in enjoyable activities | 1. Track energy patterns 2. Schedule activities during peak times 3. Create visual schedules | Proper pacing allows joints to rest and repair, reducing inflammation and preventing overuse injuries |
| Regular Medical Reviews | Comprehensive assessments including joint examination, blood tests, and medication evaluation | Prevents irreversible joint damage, enables early intervention | 1. Schedule regular appointments 2. Prepare symptom records 3. Complete pre-visit lab work | Patients seeing rheumatologists several times yearly experience better outcomes |
| Sleep Hygiene | Consistent routines and environmental modifications for better rest | Reduces pain sensitivity, inflammation, and fatigue | 1. Maintain regular sleep schedule 2. Create sleep-friendly environment 3. Limit stimulants | 80% of people with arthritis have difficulty sleeping; Poor sleep worsens pain sensitivity |
| Dental Health | Regular check-ups and proper daily hygiene routines | Reduces inflammation, prevents complications | 1. Use adapted tools 2. Schedule regular check-ups 3. Address dry mouth | Research shows RA patients have higher rates of periodontal disease and tooth loss |
| Rest/Activity Balance | Strategic alternation between movement and rest periods | Prevents joint damage while maintaining functionality | 1. Listen to body signals 2. Schedule activity strategically 3. Break activities into segments | Excessive inactivity leads to joint stiffness and muscle weakness |
| Ergonomic Tools | Properly positioned equipment and specialized tools | Reduces joint strain and pain | 1. Select supportive seating 2. Position equipment correctly 3. Maintain neutral joint positions | Studies demonstrate properly arranged workstations reduce neck, shoulder, and back strain |
| Emotional Resilience | Developing psychological strength and coping mechanisms | Improves treatment outcomes and pain management | 1. Seek support networks 2. Consider professional help 3. Practice mindfulness | Depression rates in RA patients are 3x higher than general population |
| Symptom Tracking | Documenting pain, triggers, and treatment responses | Enables pattern identification and informed treatment decisions | 1. Choose tracking method 2. Record key symptoms 3. Share data with healthcare team | Consistent tracking helps identify patterns between activities and symptom flares |
| Doctor Communication | Open discussions about treatment goals and concerns | Improves health outcomes and treatment satisfaction | 1. Prepare question lists 2. Track symptoms 3. Bring support person | 84% of patients report satisfaction with physician communication |
| Treatment Knowledge | Understanding medication categories and new research | Enables informed decision-making and better outcomes | 1. Visit trusted websites 2. Join patient groups 3. Prepare specific questions | Early treatment prevents irreversible joint damage within first two years |
| Celebrate Progress | Recognizing daily accomplishments and incremental improvements | Boosts motivation and resilience | 1. Reframe achievements 2. Create visual reminders 3. Practice gratitude | Research shows gratitude practice reduces depression rates in chronic illness |
Conclusion
Rheumatoid arthritis presents distinct challenges, yet research demonstrates that consistent, targeted lifestyle modifications can substantially enhance daily functioning and well-being. The strategies outlined above work synergistically—tobacco cessation reduces systemic inflammation while Mediterranean-style eating patterns provide anti-inflammatory nutrients that support joint health. Mind-body practices like tai chi and yoga complement medical treatments by enhancing flexibility and reducing pain perception.
Multiple strategy implementation may initially appear daunting, yet even modest changes yield measurable benefits. Studies reveal that individuals maintaining healthier weights experience slower disease progression, while those who quit smoking demonstrate improved medication response rates. Each positive adjustment creates momentum for additional improvements.
Successfully managing rheumatoid arthritis requires strategic energy conservation, ergonomic modifications to reduce joint strain, and emotional resilience building. Practical approaches such as systematic symptom tracking and open healthcare provider communication enable more personalized treatment decisions.
Rheumatoid arthritis management extends beyond symptom endurance—it involves active participation in your care through informed decision-making. Staying current on treatment advances while acknowledging incremental progress builds both confidence and motivation. These evidence-based strategies empower you to maintain control rather than allowing RA to determine your daily experience.
Living well with rheumatoid arthritis demands commitment, yet numerous patients have found that these practical approaches genuinely enhance daily functioning and overall quality of life. The path ahead may present obstacles, but these proven techniques provide valuable tools for maintaining greater comfort, independence, and hope.
Disclaimer:
This article is for informational and educational purposes only and is not intended to replace medical advice, diagnosis, or treatment. Always consult with your rheumatologist or healthcare provider before making changes to your treatment plan, medication, diet, or lifestyle. Every individual’s experience with rheumatoid arthritis is unique, and what works for one person may not work for another. The information provided here is based on current research and expert recommendations at the time of publication.
References
[1] – https://www.webmd.com/rheumatoid-arthritis/smoking-drinking-ra
[2] – https://www.webmd.com/rheumatoid-arthritis/tips-living-with-ra
[3] – https://www.hss.edu/health-library/conditions-and-treatments/managing-daily-life-rheumatoid-arthritis
[4] – https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653
[5] – https://www.arthritis.org/diseases/more-about/6-self-care-tips-for-ra
[6] – https://www.nhs.uk/conditions/rheumatoid-arthritis/living-with/
[7] – https://openworks.mdanderson.org/cgi/viewcontent.cgi?article=1086&context=sumexp21
[8] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7072747/
[9] – https://www.tandfonline.com/doi/full/10.1080/03009742.2023.2172903
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4284707/
[11] – https://www.healthline.com/health/ra-and-smoking
[12] – https://academic.oup.com/rheumatology/article/59/8/1997/5647348
[13] – https://news.harvard.edu/gazette/story/2019/02/quitting-smoking-may-reduce-risk-of-rheumatoid-arthritis/
[14] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6697238/
[15] – https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0279065
[16] – https://www.webmd.com/rheumatoid-arthritis/ra-foods
[17] – https://www.bda.uk.com/resource/rheumatoid-arthritis-diet.html
[18] – https://health.clevelandclinic.org/rheumatoid-arthritis-diet-tips
[19] – https://www.hopkinsarthritis.org/patient-corner/disease-management/rheumatoid-arthrtis-nutrition/
[20] – https://www.arthritis.org/health-wellness/treatment/treatment-plan/tracking-your-health/foods-that-can-help-ra-symptoms
[21] – https://www.healthline.com/health/anti-inflammatory-ra-diet
[22] – https://www.arthritis.org/health-wellness/healthy-living/physical-activity/yoga/tai-chi-for-arthritis
[23] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6759565/
[24] – https://www.news-medical.net/health/Yoga-and-Tai-chi-in-Rheumatoid-Arthritis.aspx
[25] – https://nras.org.uk/resource/tai-chi-for-arthritis/
[26] – https://www.health.com/condition/rheumatoid-arthritis/16-gentle-exercises-for-people-with-arthritis
[27] – https://www.healthline.com/health/8-essential-everyday-exercises-for-ra-pain
[28] – https://versusarthritis.org/news/2022/may/why-are-yoga-and-tai-chi-beneficial-for-our-bodies-and-minds/
[29] – https://www.webmd.com/rheumatoid-arthritis/yoga-poses-rheumatoid-arthritis-pain
[30] – https://www.arthritis.org/health-wellness/healthy-living/physical-activity/other-activities/best-exercises-for-rheumatoid-arthritis
[31] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7389411/
[32] – https://www.webmd.com/rheumatoid-arthritis/assistive-devices
[33] – https://www.arthritis.org/health-wellness/healthy-living/daily-living/life-hacks-tips/arthritis-friendly-kitchen-tools
[34] – https://www.hss.edu/health-library/conditions-and-treatments/assistive-devices-for-the-hand-small-joint-protection
[35] – https://www.arthritis.org.au/arthritis/arthritis-insights/living-well-with-arthritis/empowering-independence-the-benefits-of-assistive-devices-for-arthritis/
[36] – https://www.healthline.com/health/rheumatoid-arthritis/assistive-devices-for-rheumatoid-arthritis
[37] – https://www.arthritis.org.au/arthritis/arthritis-insights/living-well-with-arthritis/managing-fatigue-the-four-ps/
[38] – https://myra.org.au/article/your-feelings-tiredness/how-can-i-help-myself-fatigue
[39] – https://www.chelwest.nhs.uk/your-visit/patient-leaflets/hand-therapy/joint-protection-and-energy-conservation
[40] – https://www.ncbi.nlm.nih.gov/books/NBK384467/
[41] – https://arthritis.ca/living-well/2019/what-are-the-four-ps,%E2%80%9D-and-how-can-they-help-me-with-fatigue
[42] – https://www.nice.org.uk/guidance/ng100/resources/rheumatoid-arthritis-management-and-monitoring-algorithm-pdf-4903173613
[43] – https://www.nice.org.uk/guidance/ng100/evidence/evidence-review-e-frequency-of-monitoring-pdf-4903172322
[44] – https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/ra_guideline_summary.pdf
[45] – https://nras.org.uk/resource/monitoring-ra/
[46] – https://www.arthritisandbackpainclinic.com/2025/01/30/the-importance-of-regular-check-ups-for-people-with-rheumatoid-arthritis/
[47] – https://www.arthritisresearch.ca/rheumatology-appointment-tips/
[48] – https://versusarthritis.org/news/2023/june/how-can-i-prepare-for-a-doctor-s-appointment-if-i-have-arthritis/
[49] – https://rheumatology.org/patient-blog/how-to-prepare-for-your-rheumatology-appointment
[50] – https://www.arthritis.org/health-wellness/treatment/treatment-plan/you-your-doctor/first-appointment-with-a-rheumatologist
[51] – https://www.arthritis.org/health-wellness/healthy-living/managing-pain/fatigue-sleep/sleep-tips-for-arthritis
[52] – https://www.everydayhealth.com/rheumatoid-arthritis/living-with/sleep-remedies/
[53] – https://www.healthline.com/health/rheumatoid-arthritis/rheumatoid-arthritis-sleep-position
[54] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4495574/
[55] – https://nras.org.uk/resource/oral-health/
[56] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9960411/
[57] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9753417/
[58] – https://www.hopkinsarthritis.org/arthritis-news/5-dental-tips-for-the-ra-patient/
[59] – https://www.arthritis-health.com/blog/good-dental-care-important-those-rheumatoid-arthritis
[60] – https://www1.deltadentalins.com/wellness/conditions-and-treatments/articles/rheumatoid-arthritis-oral-health.html
[61] – https://www.health.harvard.edu/staying-healthy/exercise-advice-for-people-with-arthritis
[62] – https://hexi.ox.ac.uk/rheumatoid-arthritis/exercise-for-rheumatoid-arthritis
[63] – https://creakyjoints.org/about-arthritis/rheumatoid-arthritis/ra-patient-perspectives/overdoing-it-with-ra/
[64] – https://www.exerciseismedicine.org/rheumatoid-arthritis/
[65] – https://www.arthritis.org/health-wellness/healthy-living/managing-pain/fatigue-sleep/what-it-really-means-to-pace-yourself
[66] – https://nras.org.uk/resource/depression-and-rheumatoid-arthritis/
[67] – https://www.arthritis.org/health-wellness/healthy-living/emotional-well-being/emotional-self-care/build-resilience-to-cope-with-arthritis
[68] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7410879/
[69] – https://www.arthritis.org/health-wellness/healthy-living/emotional-well-being/anxiety-depression/arthritis-and-mental-health
[70] – https://www.sciencedirect.com/science/article/pii/S2214782921000257
[71] – https://www.everydayhealth.com/hs/rheumatoid-arthritis-treatment-management/manage-stress/
[72] – https://www.arthritis.org/getmedia/1f15caa6-cafd-4a45-a09b-3395fdba3cae/pain_trackers_ra_abbvie-2023.pdf
[73] – https://www.rheumatologyadvisor.com/news/5-best-apps-for-rheumatoid-arthritis/
[74] – https://www.webmd.com/rheumatoid-arthritis/features/best-apps-rheumatoid-arthritis
[75] – https://nras.org.uk/resource/ra-mobile-apps/
[76] – https://hqlo.biomedcentral.com/articles/10.1186/s12955-018-1035-3
[77] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10326181/
[78] – https://rheumatology.org/patient-blog/improving-communication-between-your-care-teams
[79] – https://www.the-rheumatologist.org/article/survey-patient-doctor-relationship-can-positively-affect-ra-management/
[80] – https://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/ra-treatment/
[81] – https://www.drugs.com/medical-answers/new-drugs-treatment-rheumatoid-arthritis-3512243/
[82] – https://versusarthritis.org/news/2025/april/second-stage-of-clinical-trial-for-rheumatoid-arthritis-treatment-begins-in-newcastle/
[83] – https://www.arthritis.org/news/fda-approved-olumiant-ra-treatment
[84] – https://www.verywellhealth.com/new-rheumatoid-arthritis-treatment-5221441
[85] – https://rheumatoidarthritis.net/living/tiny-wins
[86] – https://activehealthsolutions.co.uk/rheumatoid-arthritis/
[87] – https://www.webmd.com/rheumatoid-arthritis/features/rheumatoid-arthritis-keeping-a-positive-outlook
[88] – https://www.everydayhealth.com/rheumatic-conditions/how-to-have-a-healthy-relationship-with-your-rheumatoid-arthritis/
[89] – https://www.healthcentral.com/article/new-year-action-plan-for-ra






